SOCIAL MEDIA
Portuguese Medical Association's Scientific Journal
Introduction: Coronavirus has an impact on both the physical and mental health of individuals. The literature regarding the patient’s health status post-SARS-CoV-2 is still scarce with limited data on the prevalence of residual symptoms and quality of life (QoL) after the infection. The aim of this study was to understand the impact of SARS-CoV-2 on patient QoL, and remaining symptoms.
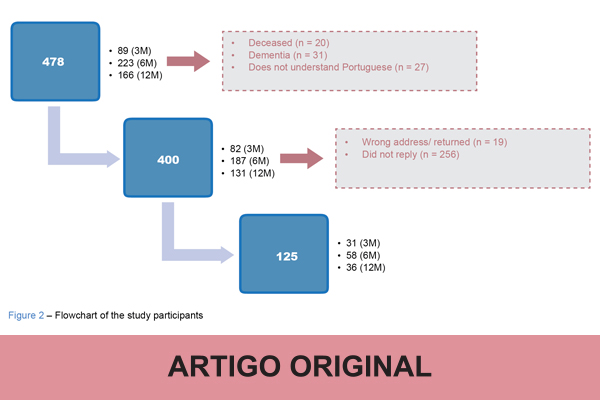
Material and Methods: Single center cross-sectional study of patients who had been admitted to our COVID-19 ward between March 2020 and March 2021. By applying a QoL questionnaire (EQ-5D-5L) we assessed the overall sample, at three time points and in different groups of patients: those admitted to the intensive care unit (ICU) and the elderly.
Results: A total of 125 participants were included in our study. Most patients who were admitted had a severe course of disease (51%), with 22% of admissions to the ICU, with 8% requiring prone ventilation, 10% experiencing thrombotic complications and 18% of nosocomial infections throughout the admission. As for persistent symptoms related with COVID-19 fog, the most frequent were fatigue (57%), memory loss (52%) and insomnia (50%). Regarding QoL, the average decrease was 0.08 ± 0.2 in the index and 8.7 ± 19 in the Visual Analogue Scale (VAS). The QoL index decrease correlated with age, chronic obstructive pulmonary disease, asthma and heart failure, and all persistent symptoms, significantly. QoL VAS correlated significantly with fatigue, mood changes, difficulty concentrating and memory loss. The decrease in QoL and the persistent symptoms remained overall stable over the three time points. The ICU group showed no statistically significant difference in QoL, but the most frequently persistent symptoms were mood changes and attention disturbances. However, the elderly experienced a worsening in QoL expressed by index (0.69 ± 0.3 vs 0.8 ± 0.2, p-value = 0.01).
Conclusion: A decrease in QoL was observed following SARS-CoV-2 infection, correlating with both chronic conditions and persistent symptoms. The lack of difference through time points of both QoL and persistent symptoms suggests a long-standing effect.