SOCIAL MEDIA
Portuguese Medical Association's Scientific Journal
Introduction: Cardiac surgery may induce acute kidney injury and the need for renal replacement therapy. It is also associated with higher hospital costs, morbidity and mortality. The aims of this study were to investigate predictors of cardiac surgery associated acute kidney injury in our population and to determine the burden of acute kidney injury in elective cardiac surgery, evaluating the potential cost effectiveness of preventing it through the application of the Kidney Disease: Improving Global Outcomes bundle of care to high-risk patient groups identified by the [TIMP-2]x[IGFBP7] used as a screening test.
Material and Methods: In a University Hospital single-center retrospective cohort study we analyzed a consecutive sample of adults who underwent elective cardiac surgery between January and March 2015. A total of 276 patients were admitted during the study period. Data from all patients was analyzed until hospital discharge or the patient’s death. The economic analysis was performed from the hospital costs’ perspective.
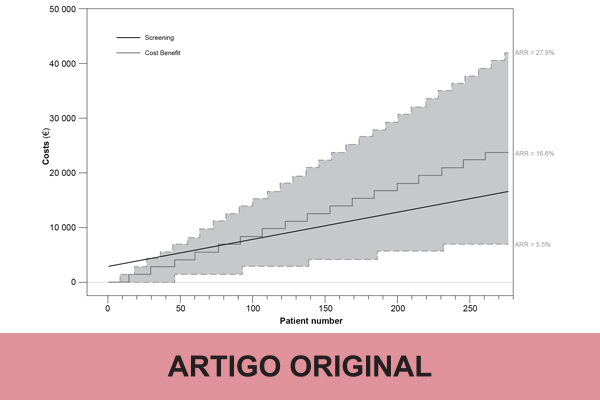
Results: Cardiac surgery associated acute kidney injury occurred in 86 patients (31%). After adjustment, higher preoperative serum creatinine (mg/L, ORadj = 1.09; 95% CI: 1.01 – 1.17), lower preoperative hemoglobin (g/dL, ORadj = 0.79; 95% CI: 0.67 – 0.94), chronic systemic hypertension (ORadj = 5.00; 95% CI: 1.67 – 15.02), an increase in cardiopulmonary bypass time (min, ORadj = 1.01; 95% CI: 1.00 – 1.01) and perioperative use of sodium nitroprusside (ORadj = 6.33; 95% CI: 1.80 – 22.28) remained significantly associated with cardiac surgery related acute kidney injury. The expected cumulative surplus cost for the hospital linked with cardiac surgery associated acute kidney injury (86 patients) was €120 695.84. Based on a median absolute risk reduction of 16.6%, by dosing kidney damage biomarkers in every patient and using preventive measures in high-risk patients, we would expect a break-even point upon screening 78 patients, which would translate, in our patient cohort, into an overall cost benefit of €7145.
Conclusion: Preoperative hemoglobin, serum creatinine, systemic hypertension, cardiopulmonary bypass time and perioperative use of sodium nitroprusside were independent predictors of cardiac surgery associated acute kidney injury. Our cost-effectiveness modelling suggests that the use of kidney structural damage biomarkers combined with an early prevention strategy could be associated with potential cost savings.