SOCIAL MEDIA
Portuguese Medical Association's Scientific Journal
Introduction: The increasing demand for emergency services has challenged healthcare systems, largely due to patients whose needs are not urgent, which account for 40.3% of admissions in Portugal.
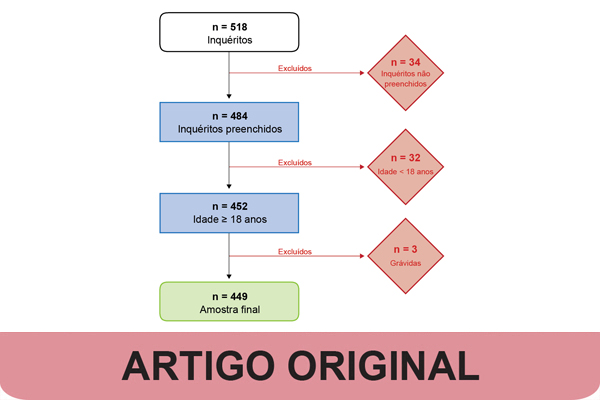
Methods: A cross-sectional study was conducted over five weeks in the emergency room (ER) of São Sebastião Hospital, Local Health Unit of Entre Douro e Vouga, involving adult patients. Data collection included the review of electronic medical records and the implementation of patient surveys in the ER. The study aimed to identify predictors of non-urgent visits to the ER, using a logistic regression model.
Results: Of the 10 333 patients who visited the ER, 12.3% were classified as non-urgent. The main reasons for seeking the ER included self-perception of symptom severity, undergoing medical tests or immediate treatments, proximity to the hospital, and the perception of higher quality care. Factors such as exemption from co-payment (OR = 0.888), proximity to the hospital (OR = 0.990), having a family doctor (OR = 0.190), knowledge of acute consultations in primary care (OR = 0.428) and telephone line SNS24 (OR = 0.089) were associated with lower odds of unnecessary emergencies. Non-urgente patients were more likely to visit the ER on weekdays (OR = 1.179) and in the morning (OR = 1.637). The probability of a non-urgent episode was 1.8% higher for each additional visit to the ER (OR = 1.018).
Conclusion: Inappropriate use of the ER is influenced by socioeconomic and behavioral factors. The exemption from co-payment was associated with a lower probability of unnecessary emergencies, raising questions about the effectiveness of this co-payment as a moderator of demand. Despite the availability of primary care, the ER was preferred during weekdays and in the morning. The association between awareness of alternatives to the ER and the presence of a family doctor with a lower probability of unnecessary emergencies highlights the need to improve patient health literacy and strengthen primary healthcare services.
Full paper available here.