SOCIAL MEDIA
Portuguese Medical Association's Scientific Journal
Introduction: The World Health Organization identified 13 critical threats to global health for the coming decade, including infectious disease prevention and antimicrobial resistance. Given the ongoing advancements in scientific evidence, it is imperative to discuss the Infectious Diseases training program. The aim of this study was to characterize and explore the respondents’ perceptions regarding Infectious Diseases training and the clinical learning environment.
Methods: A survey was developed to assess the clinical learning environment, targeting residents and young specialists who completed their training within the past five years.
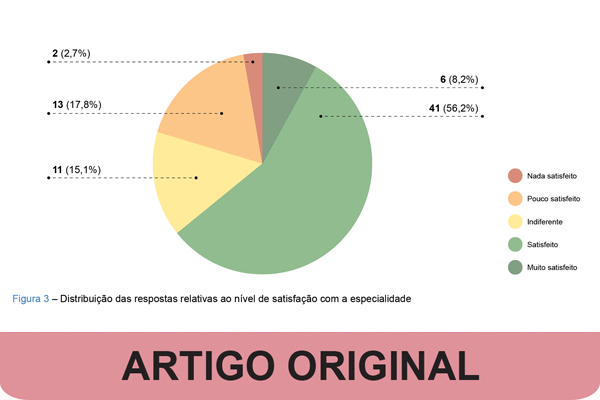
Results: The questionnaire received 73 responses, 75.3% from residents. Most respondents agreed with the duration of Internal Medicine (83.5%), Microbiology (76.7%), and General Infectious Diseases (71.2%) rotations, but considered that the Intensive Care rotation should last less than six months. The areas of Infection Control/Antibiotic Stewardship and Immunosuppression/Infectious Risk were suggested as mandatory rotations by 84.9% and 65.8% of participants, respectively. Most respondents (67.1%) considered prolonged Internal Medicine Emergency rotations beyond the first year detrimental. In contrast, 84.6% of ARS Norte participants only performed this activity during the first year, whereas 86.8% of ARS LVT participants continued, at least, until the fourth year. Regarding clinical and scientific output, ARS Norte interns reported, on average, higher numbers of weekly assisted (21.7 vs 17.1) and performed (20.8 vs 17.7) appointments, as well as higher annual participation (3.7 vs 3.1) and presentations (2.8 vs 2.4) in scientific events, published articles (1.1 vs 0.6), and weekly study hours (7.4 vs 4.5), compared with ARS LVT. The main challenges reported were a lack of dedicated study time during working hours, scientific updates, and clinical practice in Internal Medicine Emergency rotations. Regarding the evaluation of the residency program, only 2.7% agreed completely with the current exam model and 1.37% with the current curriculum grid. The majority (64.4%) of participants considered themselves at least satisfied with the specialty.
Conclusion: The results suggest a need to review the Infectious Diseases training program, include new areas of specialization, and discuss evaluation models throughout residency. Regional asymmetries were observed in emergency work, clinical and scientific output, which affect the equity and quality of training. Discussion of the Infectious Diseases training program is crucial for adapting the curriculum to current and future challenges.
Click here for the full paper (in Portuguese only)